As the world commemorates World Health Day under the theme “Healthy beginnings, hopeful futures,” many Nigerians wonder if there is truly anything to celebrate.
Despite global advancements in healthcare, the reality for millions of Nigerians remains bleak, especially for mothers and children.
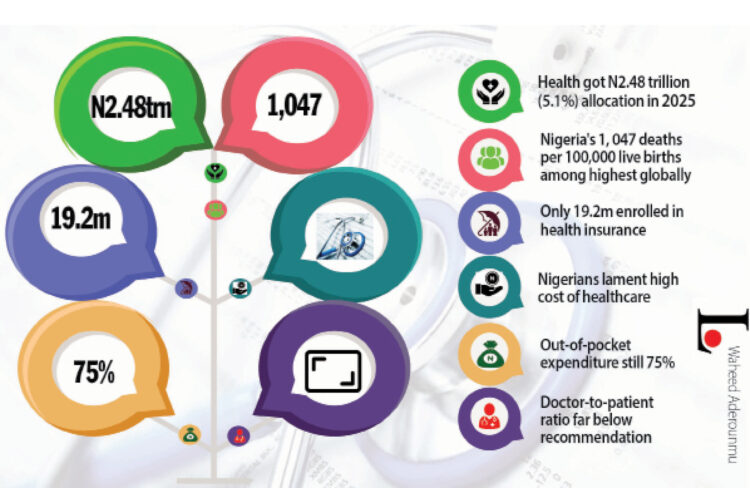
A 2023 report by the World Health Organisation (WHO) revealed that Nigeria’s maternal mortality ratio (MMR) stands at 1,047 deaths per 100,000 live births, one of the highest in the world.
Further studies shed light on the devastating ripple effect of these maternal deaths: out of 76 recorded maternal deaths in Nigeria, 64 infants were born alive. Yet, only 31.3% of these children survived beyond five years, while 68.6% did not.
Behind these grim statistics are deeper systemic issues. Healthcare in the country remains largely unaffordable and inaccessible.
LEADERSHIP’s checks revealed that many Nigerians either cannot afford hospital care or live in areas without nearby medical facilities.
Even when care is available, the country faces a worsening shortage of healthcare professionals. Many doctors and nurses continue to leave the country in search of better opportunities abroad, a trend widely referred to as the “Japa” syndrome.
Health insurance coverage is also worryingly low, leaving most citizens to rely on out-of-pocket payments for even the most basic services. For families already living on the edge, a single hospital visit can be financially devastating.
Despite policy promises, Nigeria’s health system continues to buckle under the weight of underfunding, workforce shortages, unaffordable care, and rising health inequality. In the recently proposed 2025 national budget, only ₦2.48 trillion (5.18%) was allocated to health—far below the 15 % benchmark agreed upon by African Union countries under the 2001 Abuja Declaration.
For ordinary Nigerians, the consequences are painfully real. In the Kurudu area of Abuja, a trader, Mama Mary, told LEADERSHIP that she now spends over N30,000 on malaria treatment, double what she spent just a year ago.
“I just treat myself at home with whatever I can find these days”, she said, admitting to regular self-medication.
Similarly, Mr. Ebose in Nyanya, one of the satellite towns in the Federal Capital Territory, confessed that he had stopped visiting hospitals due to the rising costs.
“I now take agbo (local herbal medicines) because I can’t afford drugs anymore,” he said.
Their stories echo the millions forced to choose between food and health.
The country’s healthcare financing remains heavily dependent on out-of-pocket payments, which account for nearly 75% of total health expenditure, far above global recommendations. Although efforts have been made to expand health insurance coverage following the 2022 National Health Insurance Authority (NHIA) Act, only 19.2 million Nigerians are enrolled as of December 2024.
While this marks an increase from previous years, it still leaves over 180 million people without health coverage.
The NHIA has promised to expand the benefit package and include vulnerable groups like pensioners, but access remains limited, particularly in rural areas.
President of the Medical and Dental Consultants Association of Nigeria (MDCAN), Prof. Mohammad Aminu Mohammed, acknowledged that while Nigeria has made “giant strides” in some aspects of healthcare delivery, critical health indices such as child mortality, maternal mortality, and under-five mortality remain deeply concerning.
Prof. Mohammad told LEADERSHIP that two-thirds of the country’s healthcare workforce is concentrated in urban areas, leaving rural communities in the lurch. He added that specialist care, often more qualitative, is also disproportionately available in cities, creating stark disparities in healthcare outcomes between urban and rural populations.
He further criticised Nigeria’s continued failure to meet the Abuja Declaration of allocating 15% of the national budget to healthcare.
“Year in, year out, we are just hovering between 4 % and 5%. We haven’t reached 6%. This lack of funding affects everything, from equipment and facilities to healthcare worker welfare,” he said.
He underlined the importance of improving incentives for healthcare workers to serve in rural areas, suggesting that improved welfare packages could help reduce the migration of health professionals abroad in search of better conditions.
The MDCAN president also highlighted the impact of inflation and economic hardship on healthcare access.
“Out-of-pocket payments remain a huge barrier. Even when people know where to get quality care, they often can’t afford it,” he said.
Prof. Mohammed advocated for expanding universal health coverage and insurance schemes to reduce the financial burden on households, particularly for chronic illnesses like heart, kidney, and liver diseases.
While stating that no country can boast of an effective healthcare system without a robust private sector, he urged the government to support private healthcare providers through tax waivers, low-interest loans, and incentives for importing medical equipment.
“These are the kinds of measures that make countries attractive for medical tourism,” he noted.
The MDCAN boss also called attention to the neglect of medical educators in discussions about expanding Nigeria’s healthcare workforce.
“We talk about increasing the number of healthcare workers, but no one is talking about those training them. We need better welfare, training facilities, and the integration of IT and AI into our medical education system,” he said.
The FCT chapter chairman of the Nigerian Medical Association (NMA), Dr Emeka Ayogu, lamented the manpower shortage in the health sector and urged the government to improve health funding.
According to him, the doctors and other health personnel are doing their best in the context of available resources.
“We have serious problems in terms of manpower, working facilities. We don’t have enough doctors on the ground. Otherwise, we are doing very well,” he said.
Dr Ayogu thanked health personnel practising in the country as he charged the government to do more by allocating more funding to the health sector and ensuring a conducive working environment and tools to enable health personnel to deliver quality health services.
“If all these are done, we will have every reason to celebrate. But for now, because of these problems, we are still not there because most skilled doctors are leaving the country in droves, which is not a very good thing,” he stated.
Amid the growing crisis, the president of the Association of Medical Laboratory Scientists of Nigeria (AMLSN), Dr Casmir Ifeanyi, condemned the proliferation of unauthorised testing facilities and urged regulators to clamp down on unlicensed practitioners.
Dr. Ifeanyi acknowledged recent efforts by the Tinubu administration to improve the health sector. However, he lamented that despite these strides, the quality of medical laboratory services remains compromised due to widespread quackery and poor regulatory enforcement.
“Healthcare is not an all-comers affair. We now have charlatans – from school dropouts to people with unrelated science degrees like zoology or biochemistry – posing as medical lab scientists. This is unacceptable and dangerous,” he stated.Also, the chairperson of the Pharmaceutical Society of Nigeria (PSN), FCT Chapter, Pharm. Salamatu Orakwelu called for sustainable drug supply chains and equitable access to medicines.
She asserted that access to essential medicines is a human right.
“Today is not just a day to celebrate health; it’s a call to action,” she stated.
Orakwelu decried the persistent health inequalities in Nigeria, pointing out that many citizens still struggle to access safe, affordable, and essential medicines. She stressed that pharmacists are pivotal in bridging this gap and reaching the most vulnerable populations, including the elderly, children, and individuals with chronic conditions.
She warned that without urgent reforms, health inequities will persist.
World Health Day is a global health awareness day celebrated every year on April 7.
US Funding Cut
External funding cuts further threaten Nigeria’s health sector, particularly from the United States. Programmes targeting HIV, malaria and tuberculosis, already fragile, are the worst hit.
A worsening crisis is unfolding in the country’s healthcare sector as hospitals and tertiary health institutions report dwindling supplies of life-saving HIV medications.
A recent investigation by LEADERSHIP revealed that facilities are yet to receive new shipments from the United States Agency for International Development (USAID), exacerbating concerns over the continuity of HIV treatment for over 1.6 million Nigerians who depend on antiretroviral therapy.
Healthcare professionals and administrators have warned that unless urgent steps are taken, the shortage could lead to severe medical complications, a rise in viral resistance, and a potential surge in new infections.
Speaking anonymously, a senior hospital administrator disclosed that the last batch of HIV drugs was received in January 2025, with the next shipment expected in April. However, due to policy uncertainties, hospitals remain in the dark about when, or if, the new supply will arrive.
The impact of the shortage is already being felt, with some hospitals suspending new patient enrollments for HIV treatment. Individuals seeking care are referred to other medical facilities where supplies remain available.
The Lagos State coordinator of the Network of People Living with HIV/AIDS in Nigeria (NEPWHAN), Patrick Akpan, refuted reports that hospitals had stopped taking in new patients.
“As of yesterday, I referred a new patient to the Federal Medical Centre in Epe, and they were placed on medication,” Akpan stated, urging patients facing treatment denial to report such case immediately.
The drugs shortage coincides with changes in U.S. foreign aid policies following an announcement by U.S. President Donald Trump about potential adjustments in international health funding.
Akpan echoed these concerns, warning that resistant HIV strains could pose a greater public health risk if treatment gaps persist.
“If people start missing doses, the virus could become stronger and more difficult to control. We must ensure that funds are released immediately to procure these medications before we reach a breaking point,” he said.
With Nigeria’s commitment to ending HIV as a public health threat by 2030, stakeholders stress the need for swift government intervention. Timely domestic funding and efficient distribution of medications are now critical to sustaining Nigeria’s progress in the fight against HIV/AIDS.
For over 1.6 million Nigerians living with HIV, the next few weeks could determine whether they continue their life-saving treatments or face devastating health setbacks.