Some medical conditions are so rare that they stay largely unknown outside of specialised medical circles. Margaria-Kalman syndrome is one such condition. It’s a rare hereditary neurological disorder classified within the broader group of hereditary spastic paraplegias (HSPs).
Though unfamiliar to many, this syndrome presents lifelong physical and cognitive challenges for those affected, requiring awareness, empathy, and tailored medical care.
First identified in the 20th century, Margaria-Kalman syndrome remains scarcely documented in medical research. Yet its distinctive symptoms and significant impact, especially when diagnosis is delayed or overlooked, underscore the need for greater understanding. In this article, we delve into the known facts about Margaria-Kalman syndrome, its symptoms, causes, and the approaches to managing this complex condition.
Understanding The Syndrome
Margaria-Kalman syndrome is a neurodevelopmental disorder that combines features of spasticity (muscle stiffness) and intellectual disability, affecting movement, coordination, and cognition. The disorder is inherited, most often in an autosomal recessive pattern, meaning a child must receive the faulty gene from both parents to develop the condition.
It belongs to a family of conditions called hereditary spastic paraplegia (HSP), which are genetic disorders marked by progressive weakness and stiffness of the legs due to damage to the corticospinal tract—the nerve pathway that sends messages from the brain to the muscles.
In Margaria-Kalman syndrome, the symptoms appear in early childhood and progress gradually. Though the severity varies, the condition typically causes both motor and cognitive impairments.
Symptoms
Children with Margaria-Kalman syndrome often present with:
Spasticity (muscle stiffness) and weakness, especially in the lower limbs
Delayed motor milestones, such as crawling and walking
Gait abnormalities (e.g., toe walking, stiffness)
Intellectual disability, ranging from mild to severe
Speech delay or language difficulties
Poor coordination and balance
Hyperreflexia (overactive reflexes)
In some cases, seizures or behavioral issues
Unlike some other neurological conditions, Margaria-Kalman syndrome does not typically shorten life expectancy. However, it can significantly affect quality of life and independence.
Because it is a rare condition, many children are first misdiagnosed with cerebral palsy or nonspecific developmental delays. Genetic testing is often required to confirm the diagnosis.
What Causes Margaria-Kalman Syndrome
The syndrome is genetic, though the exact gene mutation may vary. In families with consanguineous marriages (marriage between relatives), the risk of passing on rare recessive disorders like Margaria-Kalman syndrome increases.
Mutations affect the brain’s white matter or the spinal cord, leading to degeneration of motor neurons responsible for controlling leg movement. However, the link to cognitive deficits suggests more widespread brain involvement than in typical hereditary spastic paraplegia.
Due to its rarity, research is limited, and only a few cases have been published in medical journals. Most diagnosis is based on clinical presentation and genetic testing when available.
Diagnosis And Testing
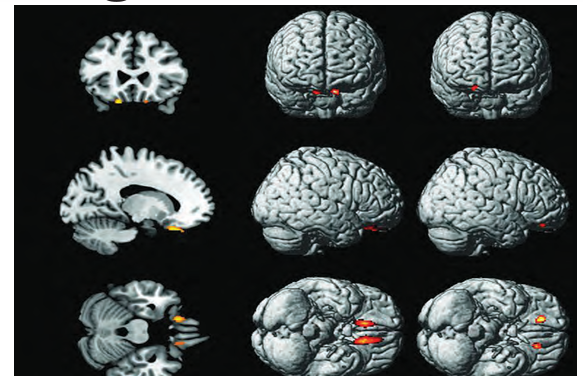
Diagnosis involves a thorough neurological examination, detailed developmental history, and brain imaging (such as MRI). Findings may show thinning of parts of the brain, white matter changes, or other abnormalities.
Key Diagnostic Tools Include:
Genetic testing, which can confirm the exact mutation
Neuroimaging, to assess structural brain differences
Cognitive assessment, to evaluate learning and behaviour
Motor function evaluation, by physiotherapists and neurologists
Because many symptoms overlap with more common conditions, early and accurate diagnosis is essential to guide appropriate therapies and family planning.
Is There A Cure
There is no known cure for Margaria-Kalman syndrome at present. However, early intervention and supportive care can improve function and development. The focus of treatment is on symptom management and helping the child achieve the highest possible quality of life.
Management May Include:
Physiotherapy to improve mobility, balance, and prevent contractures
Occupational therapy, to aid daily skills and adaptive tools
Speech and language therapy, for communication support
Special education programs, tailored to intellectual ability
Medications, such as muscle relaxants for spasticity, and antiepileptic drugs for seizures
Family counseling and support for caregivers
In some cases, mobility aids (walkers, braces, or wheelchairs) may be required as the child grows older.