The Nigerian healthcare system is ‘sick’ and under siege. The ‘sickness’ is not solely from disease, underfunding, or brain drain, but from within. There has been a silent (often loud), corrosive and destructive war among healthcare professionals that is gradually destroying the soul of the sector. The rivalry between doctors, pharmacists, nurses, medical laboratory scientists, and other allied health workers has reached a point where patients are no longer the central focus: power, ego, and supremacy battle have taken the centre stage.
We must salvage our healthcare system before it is too late and to do this, we must first heal the healers themselves. The deplorable state of healthcare delivery system in Nigeria is well documented. Our various health indices remain among the worst in the world:
- Maternal mortality rate: One of the highest globally (993 women die per 100,000 live births)
- Infant mortality rate: Over 70 per 1,000 live births.
- Life expectancy: Low at 55 years.
- Healthcare financing: Less than 5% of the national budget—far below the 15% target of the 2001 Abuja Declaration.
Nigerian health professionals are very good at their jobs but despite their noble efforts, poor service delivery, fragmented care, and low patient satisfaction persist. The health sector is held hostage by recurring strikes, leadership disputes, and professional turf wars.
How did we get to this sorry situation in the healthcare sector? What are the root causes of the Inter-Professional Wars? The answers could be as numerous as the number of people asked. Here, we can mention some factors as:
- Historical Dominance and Colonial Legacy: The British colonial health model entrenched a hierarchy that placed medical doctors at the pinnacle, relegating others to subordinate roles. This foundation has never been restructured despite the well-known advances in knowledge, training and practice in the sector.
- Ambiguities in Policy and Law: The National Health Act and schemes of service lack clear, enforceable role definitions, creating space for conflict and misinterpretation. For instance, there is a part of our statue which allow doctors to keep some medicines for immediate use and this opening has been exploited for years for them to dispense medicines in their clinics without the services of a pharmacist.
- Lack of Inter-Professional Education: Health professionals are trained in isolation. Without early exposure to teamwork, students graduate with a mindset of rivalry, not cooperation.
- Leadership Crisis: Appointments in public health institutions are often based on cadre seniority rather than leadership competence, communication skills, or strategic vision.
- Union Fragmentation: With multiple unions; NMA, JOHESU, and others who are pursuing fragmented agendas, the sector is already primed as a theatre of ‘wars’ and unity remains elusive.
- Compensation mechanism: The discriminatory salary and other compensation mechanism is one factor that has made truce and settlement a hopeless expectation.
Have we ever pondered on the price or cost of the division in the health sector? According to an African proverb, “If you want to go fast, go alone. If you want to go far, go together.” The fallout from the disunity in the sector is staggering:
- Patients suffer delayed, incomplete, or duplicated care.
- Healthcare teams operate in silos, reducing efficiency and innovation.
- Strikes disrupt service delivery and trust in the system.
- Brain drain accelerates as professionals seek more respectful environments abroad.
Rather than collaborate to solve Nigeria’s health crisis, our professionals fight over titles, job descriptions, and leadership privileges. In other climes, we have evidence of collaboration that can be adopted as the global best practices and lessons in harmony and unity. In Canada, there is a promotion of inter-professional education and integrated primary care teams. Pharmacists, nurses, and physicians are trained to collaborate from day one. In Rwanda, despite resource constraints, the country has built a resilient system through task-shifting, mutual respect, and strong public health leadership. In the United Kingdom (NHS), where many of our senior doctors were trained, leadership is competence-based. Clinical and administrative roles are often held by non-doctors, including nurses and pharmacists. In United States, Accountable Care Organizations (ACOs) incentivize team-based care, linking compensation to outcomes and collaboration. These examples show that patient-centered systems flourish when collaboration, not competition, is the norm.
It is time for us to reimagine a future in Nigeria where:
- Doctors and pharmacists will co-design patient treatment plans.
- Nurses and medical lab scientists coordinate to track recovery.
- Health information managers streamline digital health records for efficient care.
- Leadership appointments are open to all qualified professionals, based on merit, not cadre.
This vision is not only possible, but also necessary.
I will proceed to make some recommendations for the way forward:
- Policy Reforms: Review and update the National Health Act to clearly define roles and encourage collaborative structures.
- Inter-Professional Education: Revise curricula across health schools to include joint classes, team simulations, and interdisciplinary projects.
- Merit-Based Leadership Appointments: Open leadership roles to all professionals, with clear competency benchmarks for hospital management and policy formulation.
- National Health Harmony Forum: Establish an institutional platform where all unions and professional bodies can dialogue, mediate disputes, and co-create policy.
- Reward Collaboration: Introduce grants, recognitions, and performance bonuses for institutions and teams that demonstrate interdisciplinary excellence.
- Attitudinal change: It is important for all the players in the sector to change their attitudes towards each other and it should begin first, by seeing the other person as a partner rather than a competitor.
It is safe to conclude that ‘Healing Begins from Within’ as Mattie Stepanek (2002), an inspirational advocate for peace and teamwork, told us: “Unity is strength… when there is teamwork and collaboration, wonderful things can be achieved.” To heal our health system, we must first heal ourselves. The journey toward effective, efficient, and equitable healthcare in Nigeria begins with trust, respect, and collaboration among all professionals. The health sector must practice what it preaches: healing. Healing of rifts, of mistrust, of rivalry. Until we achieve this, no amount of funding, buildings, or policies will yield a truly effective healthcare system.
Let us bury the hatchet. Let us dethrone ego and enthrone empathy.
Let us remember that behind every rivalry lies a patient waiting to be healed.
Let us rise, together, and build the system that Nigeria truly deserves.
Let us heal the system by healing ourselves. The patient is waiting.
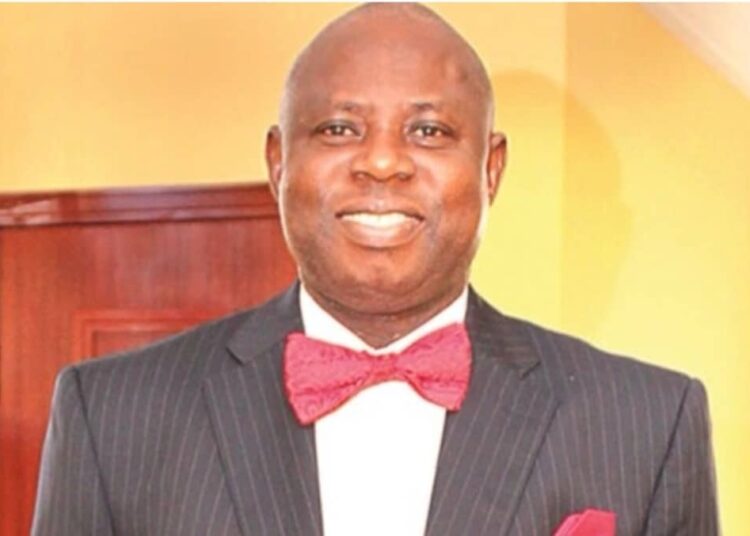
Dr. Lolu Ojo – Industrial Pharmacist, Policy Advocate, and Healthcare Reformer