While it is the dream of every couple to have a baby, they can call their own, many families seem to be so far away from realizing this dream, especially those battling with reoccurring miscarriages.
Recurrent pregnancy loss (RPL) is traditionally defined as three or more spontaneous consecutive pregnancy losses.
Studies have shown that one in seven pregnancies worldwide ends in miscarriage, and 11 per cent of women endure a failed pregnancy at least once in their lifetime.
This heart wrecking development has left many couples wondering about what could be the factor responsible for early miscarriage? A study titled: “Aneuploidy in Early Miscarriage and its Related Factors,” revealed that genetic factors are the main cause of early miscarriage.
Explaining further, the medical director, Nordica Fertility Centre, Dr. Abayomi Ajayi told LEADERSHIP Weekend that approximately, 15 to 20 per cent of clinical pregnancies will be a spontaneous miscarriage (SM) during the first trimester as a result of error in division of the cell.
“We know that in nature, about 11 to 20 per cent pf pregnancies are miscarriages. In the IVF laboratory, about 75 per cent of the embryos that we produce cannot become babies. This is so, because of the errors that happen during the time that the cells are dividing and that is one of the reasons why we are not having a 100 per cent success rate in IVF,” he stated.
The medical director, disclosed that humans are made up of the cells, adding that the cells (because they are living cells), have nucleus which contains all of the cell’s chromosomes that encode the genetic material.
In the human cell, Ajayi said the DNA is the component that is responsible for humans to transfer genetic materials to their offspring’s, adding that the DNA is packaged into thread-like structures called chromosomes. “Each chromosome is made up of DNA tightly coiled many times around proteins called histones that support its structure. Inside the chromosomes are the genes,” he added.
Speaking on the main reason for miscarriage, Ajayi said, “Cells supposed to divide uniformly into two cells, then four cells, but sometimes, problem just occur, in that we start to see mistakes happening with the division and once nature senses that mistake, it kills that embryo, leading to miscarriage. Reproduction is not efficient, but it is very specific, hence the reason we don’t have babies with two heads, because the moment nature senses the mistake, it kills that embryo.”
Preventing miscarriage
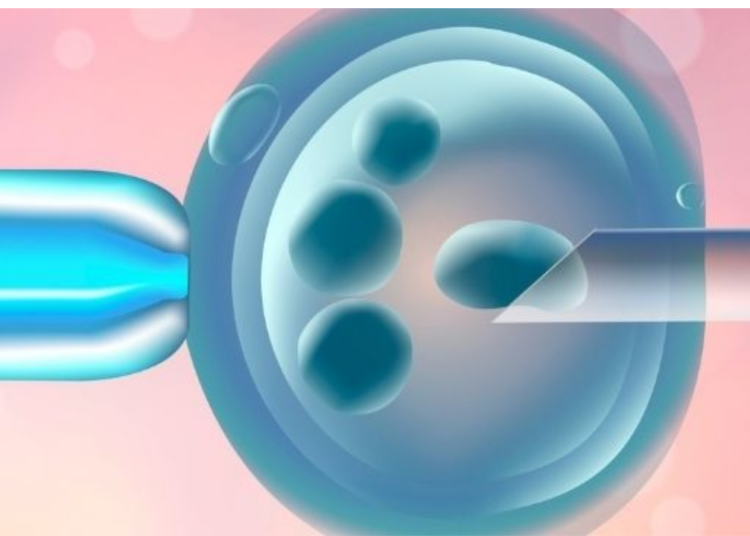
With In-vitro fertilization (IVF), it is now possible to prevent miscarriage caused by genetic factors, Ajayi said, adding that with Pre-Implantation Genetic Testing (PGT), a screening test that can be performed on embryos created via IVF to genetically analyze the embryos prior to transfer, is carried out on the embryo to test for genetic competency, before it is transferred into the uterus of the woman.
The medical director said PGT can test for aneuploidy, Structural Re-arrangement and Monogenic disorders.
Explaining further, Ajayi said aneuploidy is a genetic disorder where the total number of chromosomes doesn’t equal, leading to an unbalanced chromosome complement. This could lead to miscarriage, he added.
“With the PGT, we can now test for aneuploidy. We can also know the sex of the baby, because the chromosomes will tell whether it is XY or XX. For those who want to balance their family, PGT is the way to go,” he said.
The second test is called PGT Structural Re-arrangement, which is a PGT test done to screen for chromosomal structural rearrangements causes by balanced translocations and inversions.
“PGT can also screen for monogenic disorders, which are caused by variation in a single gene and are typically recognized by their striking familial inheritance patterns. Examples include sickle cell anemia, cystic fibrosis, Huntington disease, and Duchenne muscular dystrophy,” he said.
Couples who require PGT
The incidence of errors in chromosomes increases as the age of the woman increases, Ajayi said adding that “Studies have showed that if you have day five embryos from women who are below 35, about 50 per cent of the embryos will become babies, but because it is not only women who are below 35 years that do IVF, that is why about 75 per cent of embryos will not become babies.
“At aged 40, it is only about 15 to 20 per cent of the embryos that can form babies. From 42 years and above, the figure drops to less than 10 per cent success rate. This is the reason why doctors are always talking about age and IVF success rate.
“In essence, what I am trying to say is that women who would need to do PGT are women above 37 years, because at that stage, the percentage of embryo that cannot become babies had increased to 60 per cent. The only option is for us to test the embryos produced by these set of women, and transfer the ones that are competent, to prevent early miscarriage.”
The second group of women are those who have had a history of abnormal baby before, the medical doctor averred, adding that, “Women who have had a reoccurrence miscarriage, either naturally or through IVF would need to do PGT. Also, those with severe male factor infertility, that is those with bad sperm, would need PGT.”
How PGT is done
PGT has to be done through IVF, Ajayi said, hence the need to form embryos, thereafter, take samples from the embryos. “We used to take samples from day three embryos to see their genetic competence, but it was not efficient. Right now, we use blastocysts, that is day five or day six embryos,” he stated.
He disclosed that embryologists are trained to take the sample from the embryo without harming the embryo, adding that “They take the sample from the part of the embryo where the placenta forms. They cannot accidentally take the nose or the mouth of the baby. They take the sample (or few cells which is supposed to be a representative of the embryo), and then analyze it, to see the genetic composition of the embryo, including the sex of the embryo.
“With PGT, we can screen for genetic disorders like sickle cell disease. We can also do family balancing, in that, we transfer the embryo with the desired gender, and the one that is free from monogenic disorders. There are other diseases that you can use the PGT to screen for. About 600 diseases pattern have been discovered and all the DNA in a human being can be re-arrange. For instance, we can now, through PGT, see the sequence of albinism and congenital blindness, among others.
“The good thing about this technology is that we can only transfer the embryos that are genetically competent. This has improved the success rate of IVF to about 70 per cent. Prior to this technology, we used to select maybe two embryos by faith, and if they are not competent, it won’t form babies or may lead to miscarriage, thereby leading to many IVF cycles. But in the case where the embryos are screened through PGT, only the embryos that are competent, viable, and free from monogenic disorders are transferred into the uterus of the woman. In that way, miscarriage is lower, because miscarriage occurred when there is error with the formation of the cells.”
Speaking on the disadvantages of PGT, the medical director said, “the disadvantage with this technology is that sometimes the sample taken from the embryo may not be the representative of the embryo and as such you will not be able to get the exact result, adding that things are still improving in that regard.”